Why do we say “safer sex” and not “safe sex”? No method of protection is 100% effective – for example, viral STIs like herpes and HPV that are transmitted via skin-to-skin contact can be passed on even if condoms are used (although condoms do reduce the risk, depending how much skin area is covered). Additionally, in order for protection to work, you have to use it consistently (all the time!) and correctly. (Often, when you see different estimates of how effective a specific method is, you have to be sure to find out if the estimate is based on “perfect use” or “typical use.”)
However, given that most of us will be sexually active in one shape or form throughout our lifetimes, it’s not enough to say “just don’t have sex!” The methods listed below can help maximize the chances that you’ll enjoy sexual activity in a way that’s pleasurable AND healthy!
Internal (Female) and External (Male) Condoms
Using condoms is a fantastic way to minimize the risk of STIs. As mentioned previously, they don’t eliminate risk 100% – certain STIs like herpes and HPV can still be transmitted through skin-to-skin contact even if you’re using a condom. But overall, condoms are highly effective if you use them correctly!
Let’s talk about the different types of condoms out there. You’ve got external condoms, which are for penises (also known as male condoms), and internal condoms (also known as female condoms), which are for vaginas or anuses. External condoms can be made of different materials like latex, polyurethane, polyisoprene, and even lambskin. Just a side note, though, lambskin condoms do NOT protect against HIV, so keep that in mind.
Now, here’s how you put an external condom on the right way:
Internal condoms are another great option! These condoms are made of a soft plastic called nitrile, which is hypoallergenic. They are pretty cool because you can insert them ahead of time, before you start getting busy, which makes things more spontaneous. Plus, the inner ring of the condom can stimulate the tip of the penis during vaginal sex, and the outer ring can rub against your vulva and clitoris for added pleasure. Finally, one of the great things about using an internal condom is that you have control over your protection – you don’t have to rely on your partner to use one.
Here’s how to use an internal condom correctly:
Now, onto a few important tips:
DON’T flush condoms – throw them in the garbage! Condoms can clog things up, so to speak, and aren’t good for the environment.
DON’T use two condoms simultaneously, be it an internal and external condom, two internal condoms, or two external condoms. This can actually increase the chance of them tearing or breaking, which defeats their purpose. Remember, one condom at a time is the way to go!
Lambskin condoms do NOT offer effective protection against STIs like HIV. These condoms have microscopic pores that allow the HIV virus to easily pass through. Stick to latex or polyurethane condoms for safer sex.
Switching from anal penetration to vaginal penetration without changing the condom can actually cause an infection. So always remember, put on a fresh condom with each switch!



Other Barrier Methods
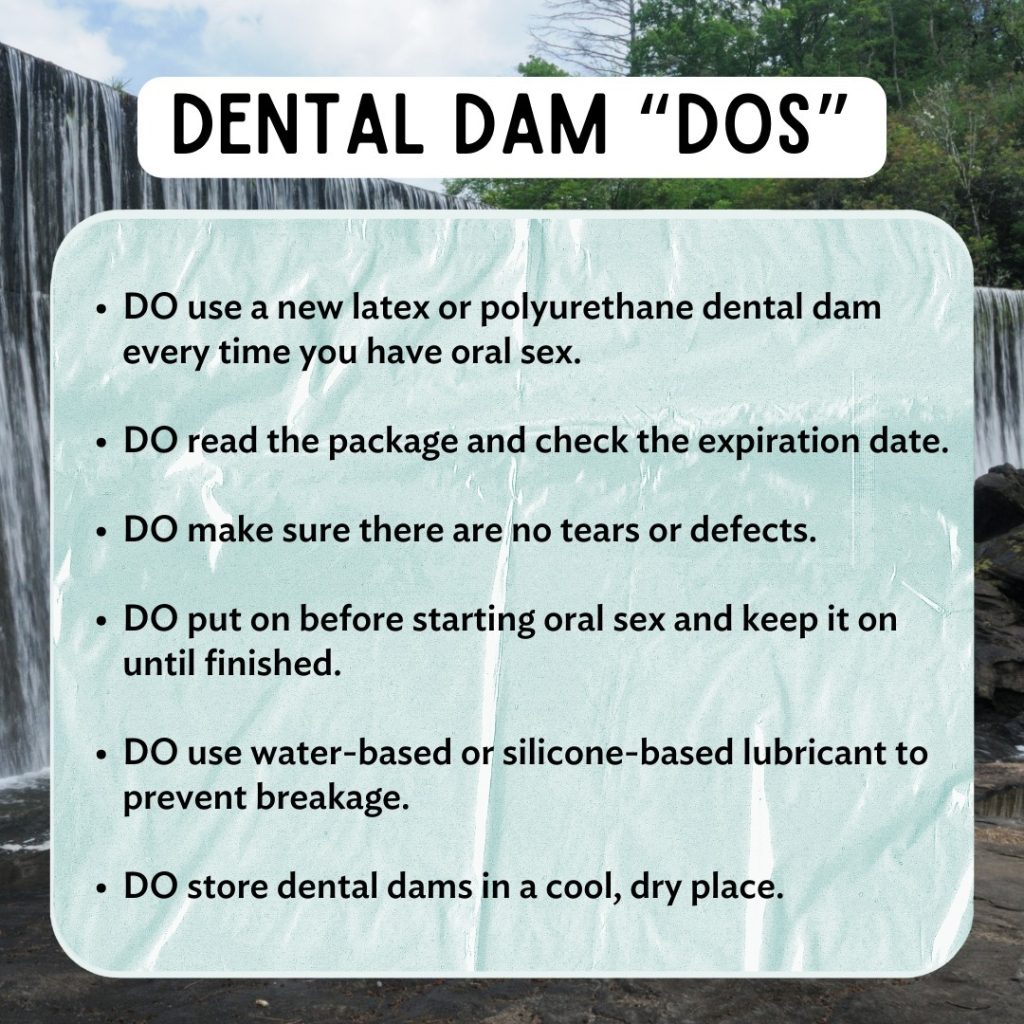
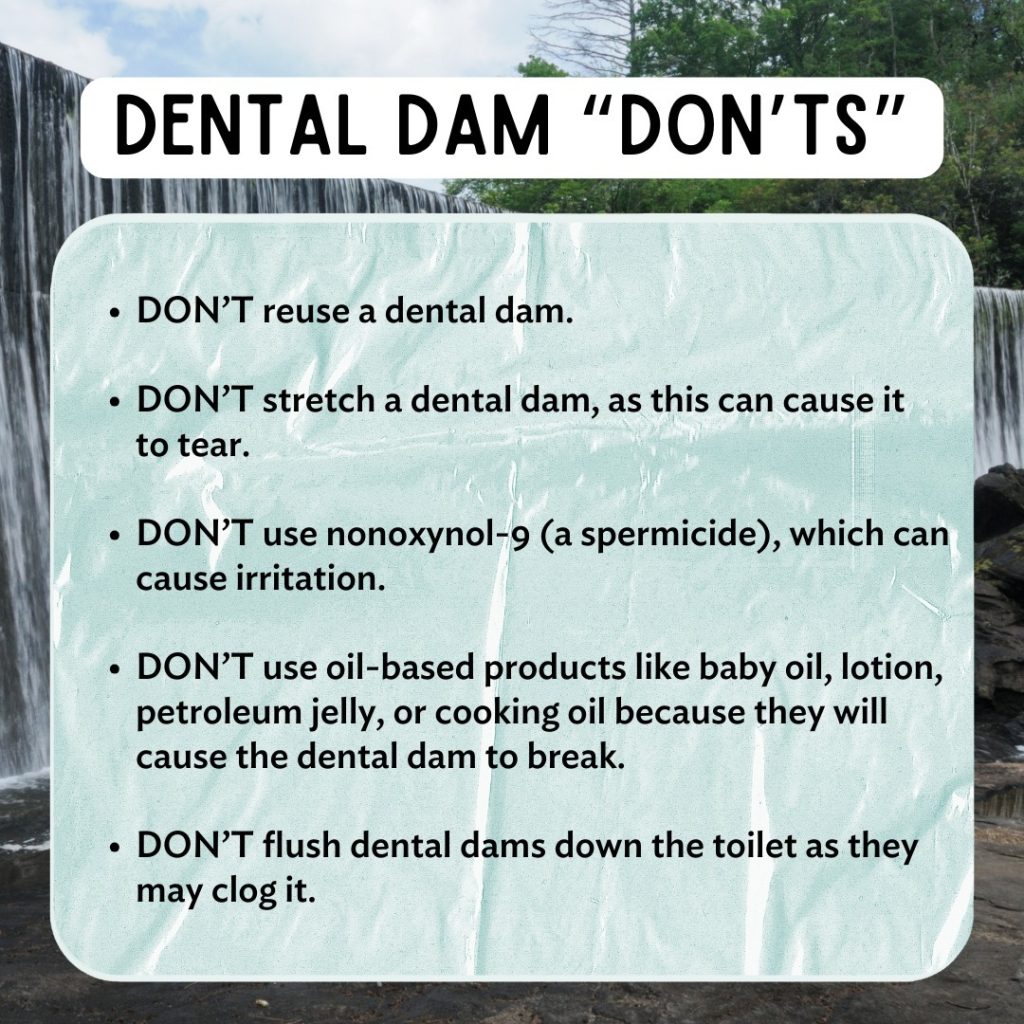
A dental dam is a square-shaped piece of latex that goes over a partner’s genitals or anus during oral sex, preventing skin-to-skin contact. Since some STIs (herpes, for example) can spread this way, dams are a good way to lower your chances of infection!
When using one, be sure the dental dam or plastic wrap covers the entire vulva (labia, clitoris, and vaginal opening) or anus and that you hold both edges so the barrier stays in place. In addition, some dental dams are latex, so be careful not to use oil-based products with them, because oil degrades latex and can cause the dam to tear. Finally, it’s important to remember to only use one side of the dental dam (if you flip it over, you and your partner will be exposed to whatever viruses or bacteria might be on the other side) and don’t reuse it.
Dental dams are sometimes not as widely available as condoms – so if you don’t have them on hand in the heat of the moment, here are some alternatives:
Lube
Using lube with condoms can make sex safer because lube decreases friction during sex which can contribute to condoms breaking. There are four main types of lube:
Try switching them up and see what works best for you! Just remember: if you have a vagina, avoid the following ingredients, since they can increase irritation and/or the likelihood of developing a yeast infection:


Pre-Exposure Prophylaxis (PrEP) and Post-Exposure Prophylaxis (PEP)
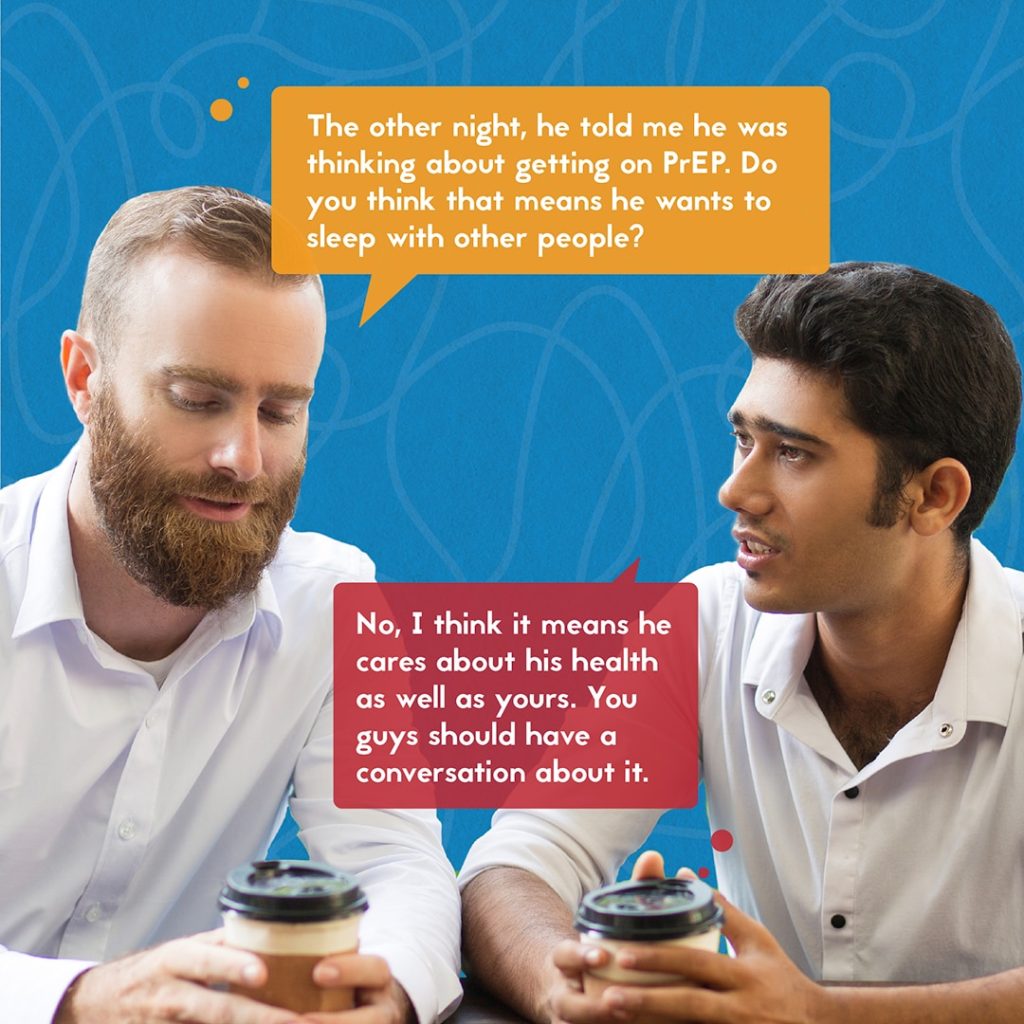
Have you heard of PrEP? It’s a daily medication for those who are HIV-negative and it’s super effective in preventing HIV infection! If taken correctly, PrEP can provide up to 99% protection against HIV. You can choose between two kinds of daily pills (Truvada and Descovy), a shot called Apretude that’s given by a provider every two months, or a shot called Yeztugo that’s given by a provider every six months (twice a year!). You can check out Lauderdale Health Center, Livingston County Department of Health, Planned Parenthood, or Trillium Health if you’re in the Rochester area. You can also find other providers through this link: https://preplocator.org/. PrEP doesn’t protect against other STIs, though, so a condom is still a good idea!
In case of potential exposure to HIV, there’s something called PEP. PEP stands for post-exposure prophylaxis and it’s a short-term emergency medication. It’s taken when you’re at risk of HIV virus “taking hold” in your body after a potential exposure (for example, if a condom rips or in cases of sexual assault). PEP needs to be started within 72 hours of exposure to be effective. You can get PEP from emergency rooms, sexual health clinics, or some doctor’s offices. Just make sure to call ahead and check if they offer PEP. You’ll usually have to take it 1-2 times a day for 28 days.
HPV Vaccine
The HPV vaccine, which is safe to take, protects against 9 strains of HPV and has the potential to prevent more than 90% of HPV-attributable cancers. The vaccine is usually given to teenagers around the ages of 11 or 12, and sometimes even as young as 9, so there’s a chance you’ve already gotten the vaccine. If you’re not sure, just have a chat with a healthcare provider or check your medical records. If you haven’t, it’s not too late – the CDC recommends vaccinations for people up to the age of 26!
For more information on the vaccine and how to get it, click here:


ART (Antiretroviral Therapy) and TasP (Treatment-as-Prevention) for Those Who Are HIV-Positive
Treatment for HIV, called antiretroviral therapy (ART), can greatly decrease an HIV-positive individual’s viral load (a measure of how much of the virus is in their system) eventually making the virus undetectable in that person’s body. This does NOT cure HIV – if that person stops taking ART, their viral load will increase and become detectable over time.
However, those with an undetectable viral load cannot spread HIV to sexual partners. This is called the “U=U” strategy – because Undetectable means Untransmittable! However, even if you or your partner are on antiretroviral therapy and have an undetectable viral load, it’s still important to use condoms to protect against other STIs.
Avoiding Sex If You Or Your Partner Have STI Symptoms or Have Been Diagnosed With a Curable (Bacterial) STI
If you’re experiencing STI symptoms, it’s best to get checked and receive appropriate treatment before engaging in sexual activity. You can find more information on various STIs and their symptoms on our website (https://wp.geneseo.edu/sexed/sexual-health-topics/sexually-transmi…-infections-stis) or visit here:
https://medlineplus.gov/sexuallytransmittedinfections.html
Keep in mind that even if you’re on medication for a curable STI, it’s possible to still spread the infection. It’s crucial to finish the entire course of treatment and ensure all symptoms are completely gone before resuming sexual activity.
Consult your healthcare provider for their guidance on when it’s safe to have sex again. For non-curable STIs like HIV and herpes, there are medications available that can help manage symptoms and greatly reduce the chance of transmission. Discuss with your healthcare provider to determine the best medications for your situation.
Lastly, it’s crucial that your partner gets tested if you’ve been diagnosed or suspect that you have an STI. Their health and well-being matter too! Thankfully, it’s possible to receive expedited partner treatment (EPT) for certain bacterial STIs. For more information about EPT, visit here:
DoxyPEP
DoxyPEP is a medicine you take after potential exposure to certain bacterial sexually transmitted infections, such as syphilis, chlamydia, and gonorrhea. It helps lower the chances of getting these infections if taken within 1 to 3 days after unprotected sex by helping to stop the bacteria from spreading in your body. The sooner you start taking it, the more likely it is to be effective!
And Finally…Get Creative!
When it comes to safer sex, there are plenty of options that don’t involve vaginal, anal, or oral sex. Get creative and explore activities like mutual masturbation, sexting, and virtual experiences through video calls (why not put Zoom to good use?). Remember, imagination can be sexy!

The information on this site is for educational purposes only. It does not replace a personal relationship with a licensed health care provider and is not intended to provide medical advice. We strongly recommend that you make your health care decisions based on your own research and knowledge of your body, in collaboration with one or more licensed health care providers.
The hosting for this website is provided by SUNY Geneseo as a courtesy, but it is not an official College publication. The statements and opinions expressed in content of this website do not represent the official position or policy of SUNY Geneseo.